Models for
Health Beliefs
A Nurturing Potential report
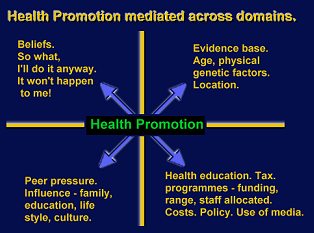
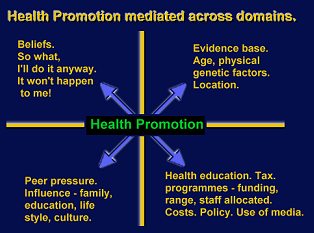
[Map courtesy of Hodges
Health Career Model]
There are a number of psychological models, designed to
predict and explain health behaviours and, in several cases, to propose
prescriptions to arrest and replace those behaviours with more appropriately
healthy alternatives.
We discussed one such model at great length in the second
issue of our magazine, in 2002 (http://www.conts.com/NPHome.html)
where we did not merely describe the prescriptions for identifying the various
stages of health behaviour, but also provided an article describing the
processes by which the authors of the Model intended it to be utilised.
The Transtheoretical Model of Change
(otherwise known as Stages of Change model)
This model, which has been applied to many areas outside that
of health, was originally promoted as a means of identifying and replacing
addictive behaviour, particularly drug and nicotine abuse.
The Health Belief Model
This model dates back to the 1950s
and was initially developed in response
to the failure of a free tuberculosis (TB) health screening
program in the United States. Since then it has been adapted to explore a
variety of long and short-term health behaviours, including sexual risk and the
transmission of HIV/AIDS.
The Model has been applied to a range of
health behaviours and classes of subject. Preventive health behaviours,
for example, would include diet and exercising to promote good health;
preventive measures such as vaccination and contraception; risk behaviours,
such as smoking and substance abuse; and clinical use by medical
professionals.
Four perceptions serve as the main
constructs of the model. As illustrated above, these are Perceived
Susceptibility, Perceived Seriousness, Perceived Benefits, Perceived Barriers.
A fifth construct of Self-Efficacy was subsequently added.
In principle, knowing what aspect
of the Health Belief Model patients accept or reject can suggest appropriate
interventions. For example, if a patient is unaware of his or her risk factors
for one or more diseases, attention can be focused on informing them about
personal risk factors. If the patient is aware of the risk, but feels that the
behaviour change is overwhelming or unachievable, the focus can be on helping
them overcome the perceived barriers
Self-efficacy refers to the extent of an individual’s belief in their abilities.
It is based on feelings of self-confidence and control, and is a good predictor
of motivation and behaviour. Recognizing and rewarding the patient for
accomplishing tasks is a useful method of helping to build the esteem that is
the basis of self-efficacy.
Self-Efficacy
This section follows on naturally from the preceding description of the Health
Belief Model to which it was added in an attempt better to explain individual
differences in health behaviours.
The model was
originally developed in order to explain engagement in one-time health-related
behaviours such as being screened for cancer or receiving an immunization.
Eventually, the health belief model was applied to more substantial, long-term
behavioural change such as diet modification, exercise, and smoking.
Developers of the model recognized that confidence in one's ability to effect
change in outcomes (i.e., self-efficacy) was a key component of health behaviour
change, and reflected a person's ability to persist
and to succeed with a task. As an example, self-efficacy directly relates to how
long someone will stick to a workout regimen or a diet. High and low
self-efficacy determine whether or not someone will choose to take on a
challenging task or write it off as impossible.
Self-efficacy affects every area of human endeavour. By
determining the beliefs a person holds regarding his or her power to affect
situations, it strongly influences both the power a person actually has to face
challenges competently and the choices a person is most likely to make. These
effects are particularly apparent, and compelling, with regard to behaviours
affecting health.
Most
people can identify things they would like to change, things they would like to
accomplish and goals they would like to achieve. A person's self-efficacy
will determine how successful they are likely to be in facing these challenges.
Although
we have introduced this subject in connection with the health model to which it
was related, it covers such a vast area of human endeavour that we propose
treating it in a complete article in the next issue of Nurturing Potential.
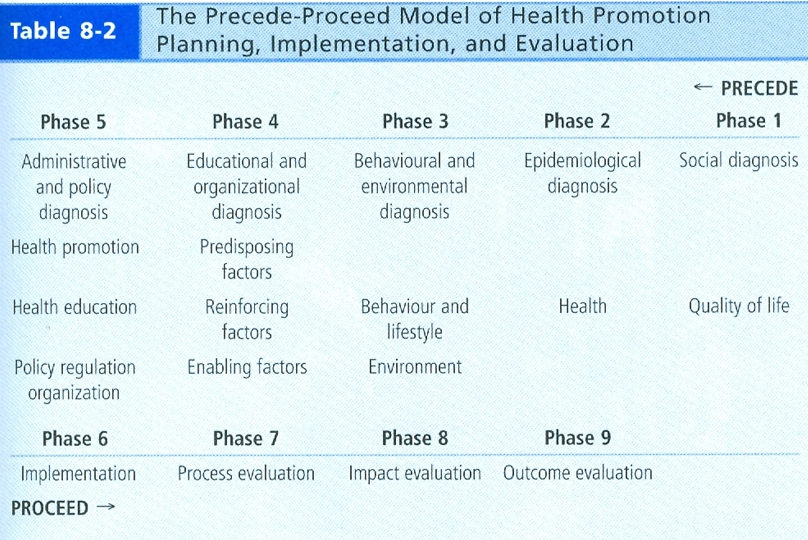
The Precede-Proceed Model
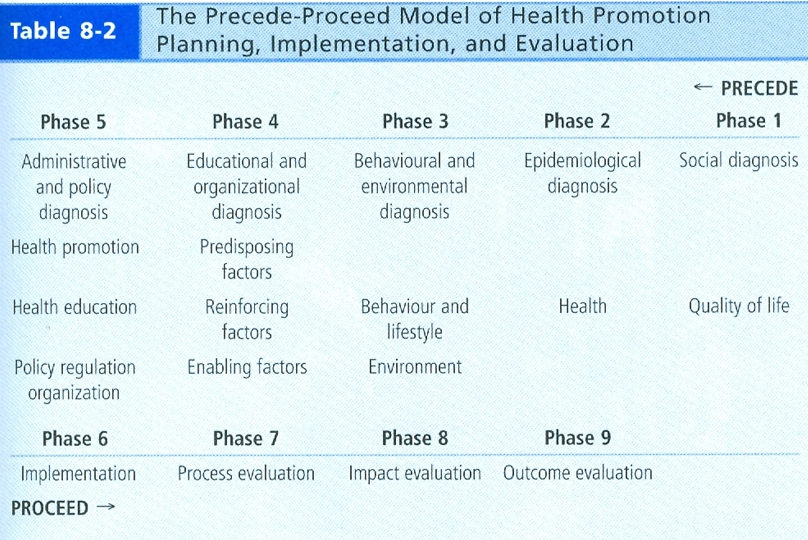
[Source: Green & Kreuter 1991 - adapted by permission by Health Promotion in
Canada]
The Precede-Proceed Model is a theoretical
framework designed to help health promotion professionals to plan, structure and
implement a programme of health promotion. It also enables the evaluation
of existing or developing programmes.
The Precede-Proceed framework for
planning is founded on the disciplines of epidemiology; the social, behavioural,
and educational sciences; and health administration. Throughout the work with
Precede and Proceed, two fundamental propositions are emphasized: (1)
health and health risks are caused by multiple factors and (2) because health
and health risks are determined by multiple factors, efforts to effect
behavioural, environmental, and social change must be multidimensional or
multisectoral, and participatory
The name derives from its two progenitors:
"PRECEDE" is actually an acronym that stands for Predisposing,
Reinforcing, and
Enabling Constructs
in Educational Diagnosis
and Evaluation. It outlines a means for accurately diagnosing and
planning a public health
programme for a targeted community. "PROCEED" is
also an acronym for Policy,
Regulatory, and Organizational
Constructs in Educational
and Environmental
Development. It
facilitates the programmes designed as a result of the
Precede process by guiding the
implementation and evaluation of those Precede
programs. While
Precede
works backward from the desired end result, attained
through the diagnostic process, to the beginning point of
the assessment process,
Proceed
works forward to implement the designed plan and to
evaluate its effectiveness.
The PPM is very much an ecological approach to health promotion. The PPM is
actually quite simple to understand once one realizes that it embodies two key
aspects of intervention: a) planning, and (b) evaluation. The PPM guides the
program planner to think logically about the desired end point and work
"backwards" to achieve that goal. Through community participation, the planning
process is broken down into objectives, step 3 sub-objectives, and step 4
sub-objectives. Conceptually, this approach to health promotion provides context
to the use of theory, with theory being applied at the fourth step. This
observation teaches a vital lesson, namely that programme planning is larger and
is a more comprehensive task compared to the subservient function of theory
selection and application.
Precede was devised in the 1970s, based on the premise that just as a
medical diagnosis precedes a treatment, so should an academic diagnoses precede
an intervention. Proceed was added in 1991 to recognise
environmental factors as determinants of health and health behaviours.
In 2005 the model was revised again to reflect the growing interest in
ecological and participatory approaches.
The Relapse Prevention Model
[Click on thumbnail for full size diagram]
This model calls for the identification of high-risk
situations for relapse and the development of solutions that prevent a
lapse (a single departure from healthy behaviour) from turning into a
relapse (a return to an addictive lifestyle).
A
technique called Relapse Prevention Planning can can make all the difference.
By thinking ahead, and by working out ways to handle the pressures that might
lead you back to your drinking, drug use or gambling, you can approach your new
life with a greater sense of confidence.
Relapse
Prevention Planning is based on the experiences and successes of many people who
have travelled the road to recovery. It recognizes that the road often has many
rough patches, and that to succeed on this road you will need a relapse
prevention plan.
A lifestyle change, however, is not easy to
make or maintain. Some people relapse
several times before new behaviour
becomes a regular part of their
lives. Thus, it is important to
learn about and use relapse
prevention techniques. First
though, it is helpful to understand the
process of relapse.
Relapse Process
At some point after making a
change, for instance stopping
smoking or attending an addiction
control group meeting, the
demands of maintaining it seem to
outweigh the benefits of the change.
We don’t remember that this is
normal. Change involves resistance.
We feel disappointed. We
forget—disappointment is a normal
part of living. We feel deprived, victimized,
resentful, and blame ourselves. We
imagine that our old behaviour would
help us feel better.
These are warning signs for a
"lapse". At this point talking
to a supportive person, or some
other form of distraction or
relaxation could help relieve the
pressure.
Cravings continue and increase.
There are so many reminders of our
old behaviour. People enjoying
cigarettes or alcohol in a movie.
The cynical or demeaning comments of
others. It is so easy to
lapse. If we recognise that
this is a natural reaction and we
have a supportive person or a plan
to distract us, we may succeed in
stopping the lapse from become a
relapse. If we allow the guilt
of our lapse to intensify, we will
almost certainly relapse.
Relapse Prevention
Preventing relapse requires that we
develop a plan that involves diversion activities,
coping skills, and emotional
support. Our decision to cope with
cravings is aided by knowing: (1)
there is a difference between a
lapse and a relapse; and (2)
continued coping with the craving
while maintaining the new behaviour
will eventually reduce the craving.
These coping skills can make the
difference when cravings are
intense:
 Ask for help from an
experienced peer and use
relaxation skills to reduce the
intensity of the anxiety associated with
cravings.
Ask for help from an
experienced peer and use
relaxation skills to reduce the
intensity of the anxiety associated with
cravings.
 Develop alternative
activities, recognize “red
flags,” avoid situations of
known danger to maintaining new
behaviour, find alternative ways
of dealing with negative emotional states, rehearse
responses to predictably
difficult events, and use stress
management techniques to create
options when the pressure is
intense.
Develop alternative
activities, recognize “red
flags,” avoid situations of
known danger to maintaining new
behaviour, find alternative ways
of dealing with negative emotional states, rehearse
responses to predictably
difficult events, and use stress
management techniques to create
options when the pressure is
intense.
 Reward yourself in a way
that does not undermine your
self-caring efforts.
Reward yourself in a way
that does not undermine your
self-caring efforts.
 Pay attention to diet and
exercise to improve mood, reduce
mood swings, and provide added
strength to deal with stressful
circumstances and secondary
stress symptoms, including loss
of
sleep, eating or elimination
problems, sexual difficulties,
and breathing irregularities.
Pay attention to diet and
exercise to improve mood, reduce
mood swings, and provide added
strength to deal with stressful
circumstances and secondary
stress symptoms, including loss
of
sleep, eating or elimination
problems, sexual difficulties,
and breathing irregularities.
SOURCES
Our descriptions of various health
models have been pieced together
from a variety of sources. For
further and more detailed
information we can direct you to the
following (non-exhaustive)
list:
Stages of Change model
detailedoverview.htm
http://www.conts.com/Self%20change.htm
The Health Belief Model
http://www.utwente.nl/cw/theorieenoverzicht/theory%20clusters/health%20communication/health_belief_model/
http://www.ohprs.ca/hp101/mod4/module4c3.htm
http://heb.sagepub.com/content/11/1/1
http://midrangeborrowedtheory.weebly.com/critical-elements-health-belief-model.html
The Precede-Proceed Model
http://www.lgreen.net/precede.htm
http://envirocancer.cornell.edu/obesity/intervention101.cfm
http://ctb.ku.edu/en/table-contents/overview/chapter-2-other-models-promoting-community-health-and-development/section-2
The Relapse-Prevention Model
http://www.albertahealthservices.ca/2485.asp
http://www.tgorski.com/gorski_articles/developing_a_relapse_prevention_plan.htm
http://www.recovery.org/topics/relapse-prevention/
http://www.addictionsandrecovery.org/relapse-prevention.htm
http://psychcentral.com/lib/relapse-prevention/000273
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3163190/
![]() Ask for help from an
experienced peer and use
relaxation skills to reduce the
intensity of the anxiety associated with
cravings.
Ask for help from an
experienced peer and use
relaxation skills to reduce the
intensity of the anxiety associated with
cravings.
![]() Develop alternative
activities, recognize “red
flags,” avoid situations of
known danger to maintaining new
behaviour, find alternative ways
of dealing with negative emotional states, rehearse
responses to predictably
difficult events, and use stress
management techniques to create
options when the pressure is
intense.
Develop alternative
activities, recognize “red
flags,” avoid situations of
known danger to maintaining new
behaviour, find alternative ways
of dealing with negative emotional states, rehearse
responses to predictably
difficult events, and use stress
management techniques to create
options when the pressure is
intense. ![]() Reward yourself in a way
that does not undermine your
self-caring efforts.
Reward yourself in a way
that does not undermine your
self-caring efforts. ![]() Pay attention to diet and
exercise to improve mood, reduce
mood swings, and provide added
strength to deal with stressful
circumstances and secondary
stress symptoms, including loss
of
sleep, eating or elimination
problems, sexual difficulties,
and breathing irregularities.
Pay attention to diet and
exercise to improve mood, reduce
mood swings, and provide added
strength to deal with stressful
circumstances and secondary
stress symptoms, including loss
of
sleep, eating or elimination
problems, sexual difficulties,
and breathing irregularities.